A volatile physician staffing market puts a premium on flexibility.
Two years ago it looked like a fundamental change had taken place in the Emergency Medicine job market in the United States. For the first time in memory, there appeared to be more doctors than jobs.
A few trends had converged. First, ER volumes plummeted in the first summer of the pandemic, and thus physician staffing groups hired fewer recent graduates from residency to staff emergency departments. Meanwhile, the number of EM residency programs had been steadily climbing for years, meaning there were more graduates than ever. At the same time, physician groups increased their reliance on APPs.
The result was a kind of panic. In 2021, the American College of Emergency Physicians convened a task force to study the future of the EM physician workforce. The task force produced a report, and the resulting Emergency Medicine Physician Workforce: Projections for 2030 still looms large in the minds of many in the industry.
And yet, since then, trends have reversed themselves. We are again in a tight job market for Emergency Medicine physicians. The decades-long challenges of finding the right physicians to work at rural or difficult-to-staff sites remain.
This year, the biggest news story in the Emergency Medicine job market was that more than 500 residency slots went unfilled. Some took this to mean that medical students were losing interest in going into Emergency Medicine. Yet there are 1,000 more residency spots available than there were ten years ago. In other words, we are still minting many more new Emergency Medicine physicians than we used to.
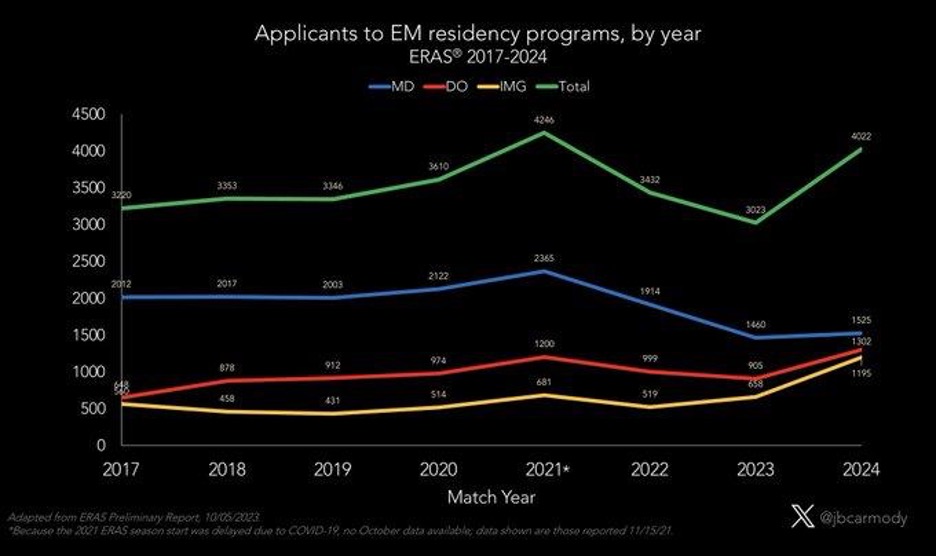
Dr. Bryan Carmody, a pediatric nephrologist and associate professor at Eastern Virginia Medical School, crunched ERAS data to show that applications to EM residency programs actually spiked dramatically this year, reversing a two-year downward trend:
The data shows a 33% increase.
What happens in the future is yet to be seen. Any predictions about the long-term trends for the EM job market should be taken with a grain of salt.
Yet, the implications for hospitals and health systems are clear, especially those that have had difficulty staffing their emergency departments in recent years. The answer to this kind of volatility is flexibility.
Emergency Medicine has certainly become a more difficult job post-COVID. Managing the patients is harder. Financial pressures felt by physician staffing groups are making themselves felt at the bedside. The hospitals that will be most successful in weathering these trends are those that partner with groups flexible enough to handle whatever comes their way, whether it’s a glut in the market or, as has been more historically the case, a significant shortage.
“The reality is there’s a lot we just don’t know,” says Core Clinical Partners CEO, Dr. Boykin Robinson. “But Core’s agility and adaptability has proven indispensable” in the ever-changing landscape.