Lessons learned as I started Core Clinical Partners
Greetings from Atlanta.
Welcome to the first issue of a monthly newsletter we’re launching here at Core Clinical Partners. I plan to send these reports out on the first every month, and I plan to write about all things related to the business of emergency and hospital medicine, unscheduled acute care, and the evolving healthcare landscape from a physicians services group point of view.
I expect that will turn out to be a pretty wide net, as our business has expanded into a lot of areas since many of us trained. Physicians services groups (the good ones) are expected to be true partners to their hospital clients.
That’s what’s behind our name, Core Clinical Partners. Because partnership is core to what we do. But in this newsletter I’m going to try to go deeper than just some marketing copy thrown onto a one-pager. I will strive to be more transparent than what you might see from other groups in the space. And finally I will use this newsletter as a tool to communicate lessons learned as we continue to grow and evolve as a business.
The first lesson, which I learned through many fits and starts over the first three years since Core was founded, going from zero to 35 contracts in 13 states is this: there is no one size fits all way to be a good partner.
How I started Core (With a Hospital Bankruptcy)
A lot of folks will tell you why they started a company, and then throw a bunch of “values” at you. I’ll get to that soon enough.
As an introduction, though, the how is a bit more interesting.
Basically, I started Core in the aftermath of a hospital bankruptcy.
1. $4.2 million for a hospital
In 2015, Hutcheson Memorial Hospital in Fort Oglethorpe (a suburb of Chattanooga) was failing. It had been independent, and probably should have sold or merged much earlier.
At the time, I was a divisional president for ApolloMD. We’d taken over management of Hutcheson’s emergency department that past June, and we’d watched as it went into bankruptcy, went to auction and the bank rejected several offers to buy the place.
The issue had been the surgical center attached. As it turned out, the bank had been over-valuing it. Then we saw someone come in with an offer to buy just the hospital for $4.1 million, and we thought to ourselves, “Well, what if we offered $4.2 million?”
And just like that — all of a sudden we owned this gigantic shuttered building on 45 acres.
2. Something completely different
Hutcheson’s ED had been seeing about 20,000 patients annually — a healthy volume for a small hospital. The problem was the rest of it.
Between me and Jessica Long, who was my Sr. VP of Operations at the time (she’s now Core’s Sr. VP of Strategic Initiatives), we had our hands full. She became CEO of the new hospital, which would be named Cornerstone, and I became the Chairman of the Board.
In the span of a few days, we held a job fair, and hired everyone we needed to get the lights turned back on and start seeing patients.
If you Google news about the event you might come across a report from the Chattanooga Times Free Press describing the re-opening: “After a bankruptcy court judge approved ApolloMD’s offer to buy Hutcheson last week, the company’s employees began to prepare the hospital to see patients again, ripping plywood off its windows and removing bags that covered Hutcheson’s signs.”
It was exciting because it was something completely different. I’d been in physician services my whole career, and now all of a sudden we were hiring environmental services and facilities managers and nurses and respiratory techs, and thinking about how we could cost-effectively run a micro-hospital within a larger hospital building.
3. The business opportunity
As the Times Free Press wrote in the same article: “[ApolloMD] has not yet released a strategic plan for how it will make the hospital economically viable, especially after years of losing money and receiving negative attention.”
And yet, we did begin to turn things around. We took a place that had been hemorrhaging money, and turned it into a well-managed facility that was an attractive acquisition opportunity. We improved its reputation, had a growing patient population, and had laid the groundwork for a hospital group to come in and take it to the next level.
Which is exactly what happened two years later when Catholic Health acquired it. Today, what had been a bankrupt facility with plywood over the windows is named CHI Memorial Hospital Hospital Georgia. It has 36 acute care inpatient beds and has lab, radiology, pharmacy, and a range of outpatient and surgical services.
The business opportunity for me came just after we sold it. Apollo was still managing the hospital’s emergency department, but we also managed a nearby competitor. Pretty soon the competitor’s CEO called me up: “You’re now running the ER of a competitor,” he said. “And I need you to be my partner in this market.”
It was unfortunate, but it’s a reality in our business: hospitals compete for patients, and sometimes physicians services groups get stuck in the middle. We needed to drop the contract with CHI. I connected Jessica, who was still CEO, with some doctors who I expected would take over the contract. Instead, they suggested I take over the contract — and start a new physicians services group in the process.
4. My first theory of partnership
At first, it felt kind of like a crazy proposition. I would go from running more than $200 million in business with dozens of contracts in multiple states to $3 million in business with one contract.
In the end, though, it wasn’t a hard decision. Earlier that year, in 2018, I had already decided to go back to school to get an MBA. This was the opportunity to put my desire to build something to the test.
And, I had a theory about how to build it: true, transparent ownership at the contract level.
I wanted to build the entire company around this idea. The other, big CMGs often had a version of partnership, or a version of ownership, but not what I considered real and true and transparent.
To me, ownership meant K-1 — the form you file with the IRS to declare your ownership interest in a partnership. Transparent meant owners could see the financials, and so could hospital partners.
Finally, putting ownership at the contract level would mean our partners were invested in that site, as opposed to a corporate entity based somewhere else. My thesis was that if you’re going to get a doctor to work three extra shifts to avoid locums coming in, then the doc has to care about that specific contract.
At least: that was the theory.
5. Theory meets reality & lessons learned
After CHI, two of our first contracts came from a group called Legacy Physician Partners out of Nashville. The group was imploding. They couldn’t make payroll, so different contracts in different parts of the country were turning over to other groups with varying degrees of success. Some physicians were not paid at all.
Meanwhile, Core went in to two Legacy sites and offered to cover the payroll of the physicians and APPs who had been working there. They were all very aware their company was going under, and grateful to at least be getting their paycheck.
I told the clinicians about our partnership model. But the reality was the partnership at the moment was that Core just made payroll without any revenue, and there were a lot of things that needed to be fixed before the contracts would be profitable and for the partnership to be meaningful.
I’d learned my first, and still one of my most important lessons: every situation is different.
As new opportunities arose for Core to grow, I realized the point of contract-level ownership isn’t the K-1 — it’s alignment. There is no one size fits all way to do partnership, whether that’s with physicians at a new site or with a hospital partner in a new region.
What is important is physician alignment. The docs who work in a community must have their incentives aligned with the goals of the hospital serving that community.
But the reality on the ground is that there are a lot of different ways to get there. Which one you choose depends on the people involved, the situation at the hospital, the financial situation, and many other factors.
All hospitals have similarities, and all emergency departments have similarities, but ultimately every situation is different. That recognition, more than any theory about ownership or partnership, is how Core has been allowed to grow and be good partners.
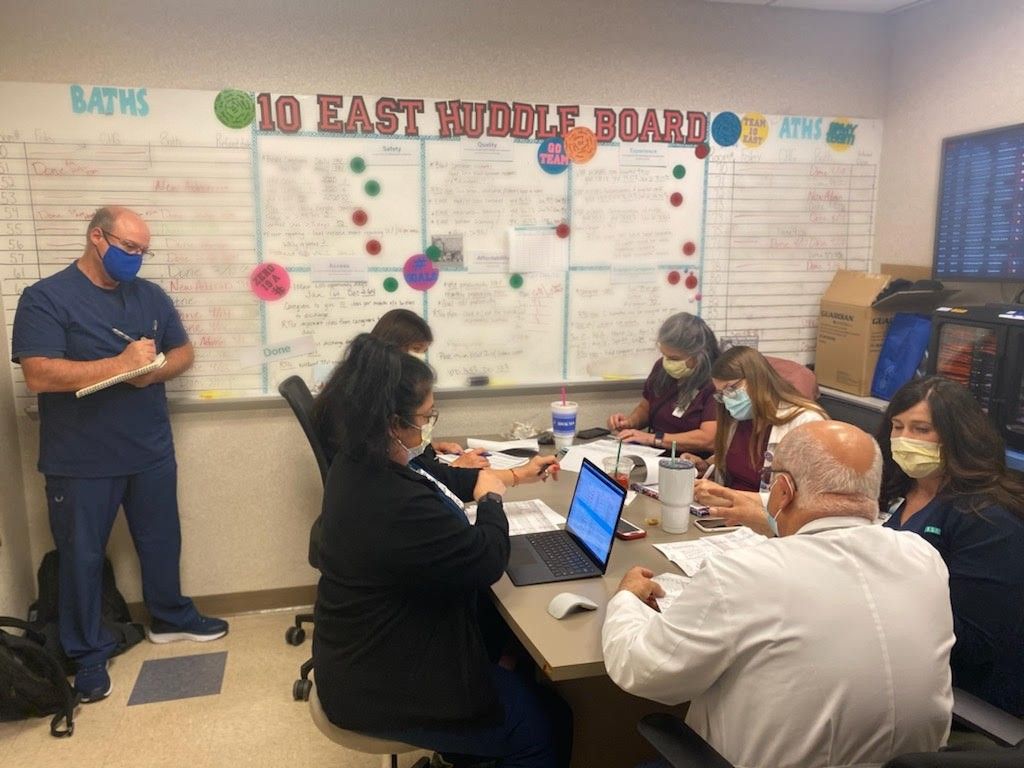
Boots on the Ground: Oklahoma City
One thing our commitment to partnership allows is for extended, boots-on-the-ground presence to work on process improvement.
Last month, Core’s VP of Clinical Operations, Mark Canada, visited our partner INTEGRIS Baptist for nine straight days. There, he helped the on-site hospitalist teams implement a new geographic rounding model.
Mark came to us from Envision, and has a long track record of successful process improvement there. If you want to learn more about his approach, we did an extensive Q&A with him about his approach to clinical operations.