TRANSFORMING A SEVEN SITE HOSPITALIST SERVICE: CREATING CAPACITY AND $100 million in REVENUE
THE CHALLENGE
Despite evidence that Hospitalists reduce the length of stay and improve quality, a Hospitalist program spanning seven hospitals in a large metropolitan area was unsuccessful. Incremental fixes such as hiring additional physicians and geographic rounding did not decrease the length of stay. Unnecessarily long inpatient stays limit bed availability which results in increased Emergency Department Length of Stay (LOS), boarding, and a limited ability to accept transfers.
Contributing further to the challenge was a culture needing more mutual trust, transparency, and a focus on improvement. As a result, the collaboration between the Hospitalist group, medical staff, and senior leaders stagnated, and thus a change in the hospitalist group commenced. An initial key challenge for the key stakeholders of the system leadership (CEO, CNO, CMO) and Core
Acknowledging the need to leverage diverse strategies and collaborative approaches, key stakeholders initiated practices to imbue a culture of listening while operating with clear goals and implementing incentives focused on performance improvement. In addition, innovative forums promoted shared decision-making and transparent communication to improve the practice environment and care systems.
Working as a collaborative team, the stakeholders have a strong sense of purpose and strategic insight. And the impact is measurable in decreased length of stay and readmission rates.
THE SOLUTION
Geographic Rounding and Unit-Based Interdisciplinary Rounds
Core Clinical Partners swiftly implemented its own process for executing a sustaining geographic rounding program at the two larger facilities, giving a cohort of the same type of patients to the same doctor. This practice improved patient-doctor relationships, nurse-physician relationships, and increased efficiency. The move to geographic rounding also facilitated unit-based interdisciplinary rounds, fostering greater collaboration among the care teams.
Admission Team Support
Admission team support was matched to admission loads 24/7, dramatically reducing the number of patients held in the Emergency Room. Before this change, there were often 10-20+ patients waiting in the ER every morning. This number was reduced to zero most days and this faster transfer from ER to the inpatient nursing units promoted quicker treatment and discharge times.
Standard Transfer Acceptance Protocol
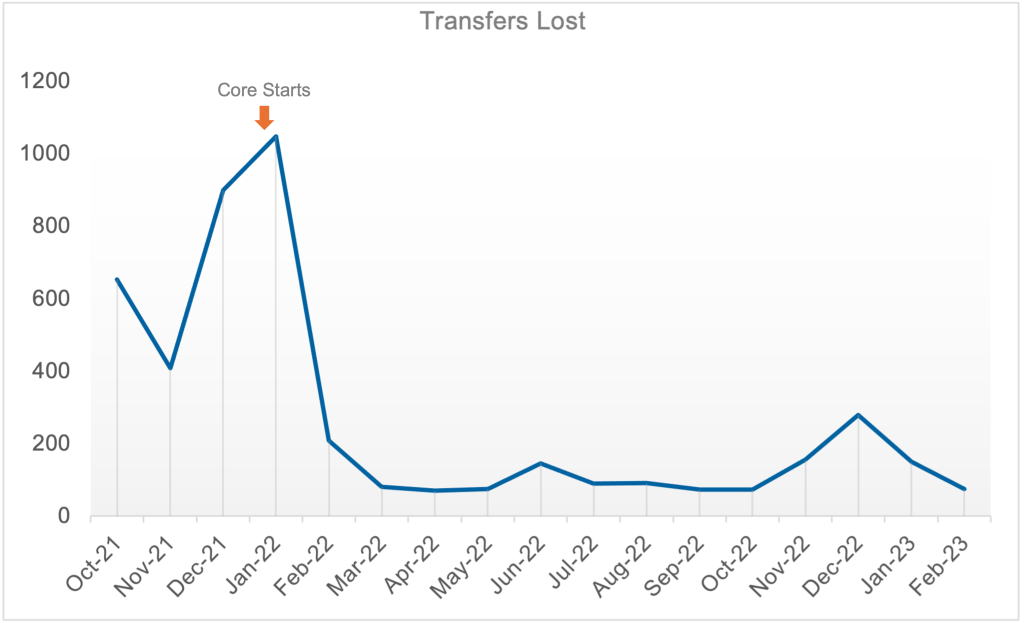
Key stakeholders established a standard transfer acceptance protocol, alongside specialty-specific transfer acceptance subprotocols, to promote prompt acceptance of transfers across the system. By developing algorithms for the auto-acceptance of patients, the team significantly minimized the previous back-and-forth communication that often resulted in patients being accepted at competing facilities.
Advanced Utilization of Epic Chat
Communication was enhanced by encouraging the use of Epic secure chat, an available technology that had previously gone mainly unused. Epic’s chat allows doctors and Advanced Practice Providers (APPs) to communicate securely about patients, download charts, and even put in orders, while remaining HIPAA compliant. This direct communication method cut down on time delays, making patient care more efficient.
Provider Coaching and Commit-to-Sit Program
Provider coaching was introduced using a patient experience communication model, including a commit-to-sit program. This program encourages doctors to sit down with patients during their rounds, promoting better communication and patient satisfaction.
Data Management and Partnership
The team focused on data management to understand volume spikes and make necessary adjustments to how care is delivered. Using Core Analytics, a unique volume analytics tool, hospitalists and senior leaders were able to analyze LOS and provider specific data and make informed decisions or adjustments to practice. Moreover, Core Clinical Partners emphasized the importance of partnership, assigning a Director of Operations (DOO), Director of Clinical Operations (DCO), Practice Coordinator, and a Medical Director to each site for onsite administrative support. This onsite leadership presence further promotes daily collaboration and provides a visible reminder of why patient care is important.
THE RESULT
-
Discharge efficiency improved, leading to a 0.69-day reduction. With approximately 2,500 discharges per month and a per-patient revenue of $800, this saved the hospital approximately $15.6 million in annual revenue.
-
Transfer acceptance increased by 99.2%, from 485 In October of 2021 to 966 In October of 2022. Consequently, the number of declined transfers decreased by 79% year over year due to Increased bed capacity. THIS GENERATED AN ADDITIONAL REVENUE OF $86.3 MILLION.
-
The 30-day readmission rate saw a significant decrease of 12%, putting the system on track for 300 fewer 30-day readmissions in 2022.
-
-
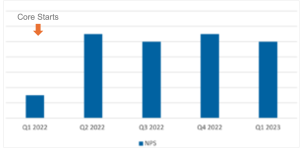
A 6-point improvement was noted in the Net Promoter Score (NPS), surpassing the hospital system’s goal. This increase can be attributed to the provider coaching, commit-to-sit program, and improved communication facilitated by the Epic chat system.
These strategic actions led to notable advancements in patient care, operational efficiency, and financial performance for a multi-site hospital system. The commitment to modernizing practices, improving patient-physician communication, promoting nurse-physician communication, and optimizing data management demonstrates the transformative potential of an aligned strategy. Furthermore, casting vision and engaging stakeholders at the early stages of a process, including clinician selection and onboarding, allows senior leaders, physicians, and other clinicians to follow its progress and develop a sense of shared ownership; ultimately building momentum that pulled others in as the strategy comes to fruition.